This post may contain affiliate links. Please read our disclosure for more info.
"It was just bad luck, so don’t blame yourself,” my oncologist explained.
I knew in my gut it wasn't "normal" for someone in their 20s to develop breast cancer. Not that getting cancer at any age is acceptable.
I thought hearing my oncologist's explanation of why I developed breast cancer would put everything in perspective. But blaming this on bad luck seems so -- unscientific.
I had a burning question ever since I was diagnosed:
Is breast cancer really random?
Having a background in science, I knew there’s more to getting breast cancer than bad luck.
The Incidence of Breast Cancer is Rising
October is breast cancer awareness month and the “pink” campaigns will soon surround us promoting early detection, breast screening and seeking donations to fund a cure.
What’s really hard to believe is that we have yet to see an improvement in the incidence of breast cancer.
Have you ever noticed the lack of prevention campaigns for breast cancer?
It’s crazy to think that after billions of dollars spent on breast cancer research, there’s never been any major breast health campaign. There’s lots of awareness in checking your breasts and being wary of early signs and symptoms.
But isn’t stopping it altogether better than catching it early?
So what do the experts tell us about the cause of breast cancer?
If you haven't already checked out any of the respected breast cancer organisation websites, they all state risk factors that increases the chances of a woman developing breast cancer (see table below).
These risk factors are divided into UN-MODIFIABLE (those that you can't change) and MODIFIABLE (those that you can change). There’s also evidence that a few protective factors decreases the chances of a woman developing breast cancer. Check out some of the most common risk factors below.
Those risk factors seems pretty straightforward.
But in simply visualising the risk factors as neat bullet points, we’ve lost appreciation of the intricacy of what causes breast cancer.
There is a more complex picture.
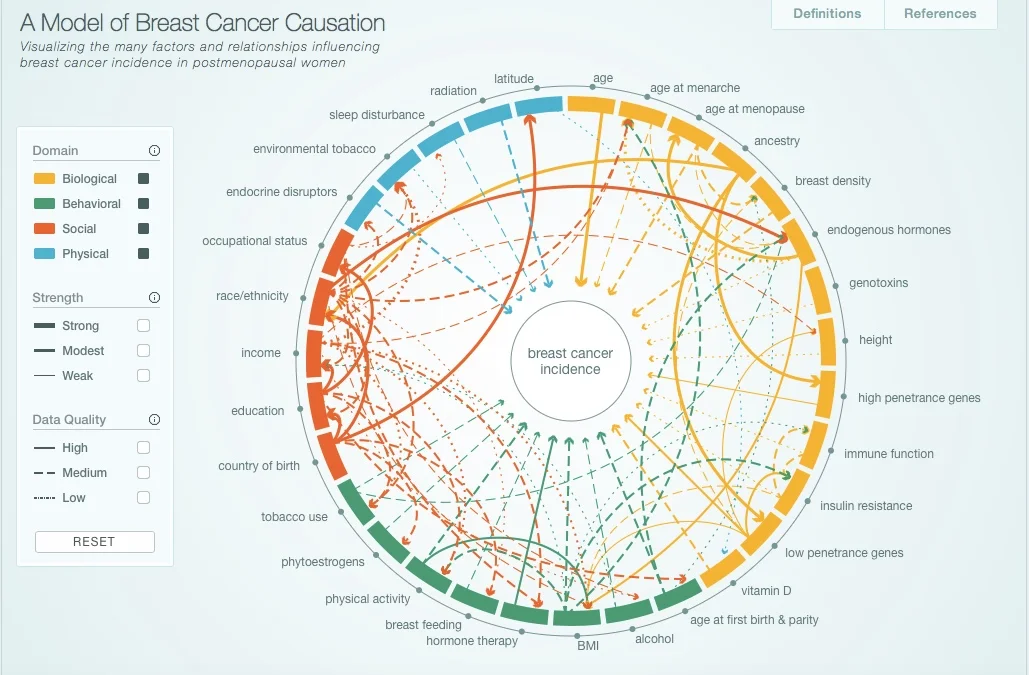
We can begin to understand this in the model of breast cancer causation created by Robert Hiatt from the UCSF.
In this model, the development of breast cancer is an interplay of risk factors that fall under four major categories:
Biological
Behavioural
Social
Physical
The research gathered has been from postmenopausal women and are currently working on a similar model for premenopausal women.
I recommend you click through to their website to play around with their interactive model to educate yourself on how one risk factor are connected with other risk factors.
Interactive Model of Breast Cancer Causation - http://cabreastcancer.org. The full research article was published in journal Cancer Epidemiology, Biomarkers and Prevention can be found here.
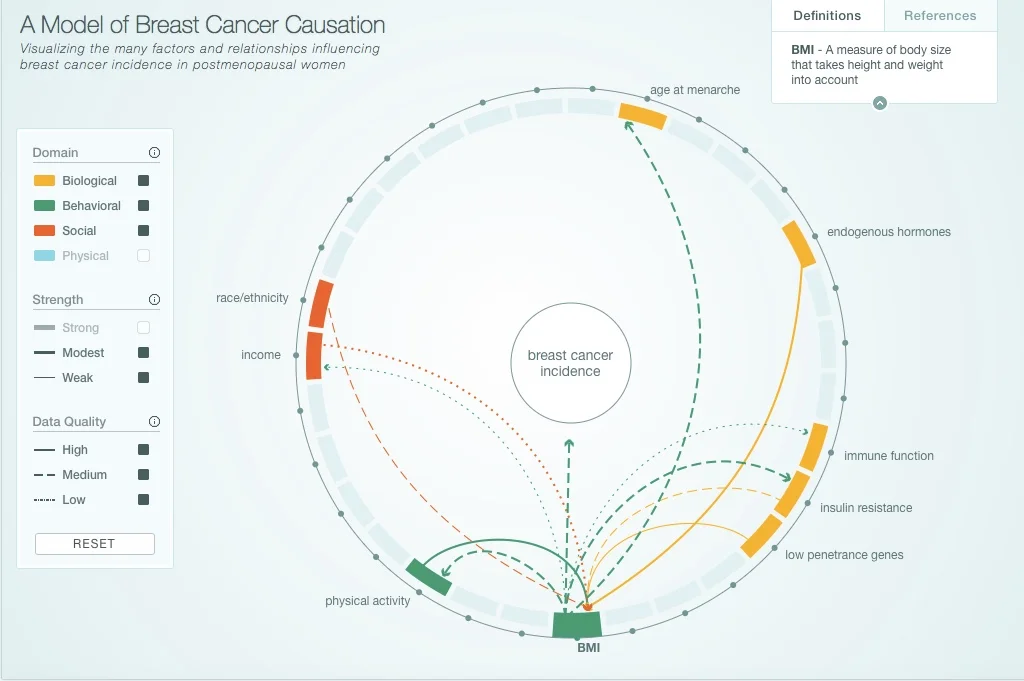
If you click on just one risk factor, for example BMI (see screenshot below) - it displays any relationships with other risk factors:
physical activity
race/ethnicity
income
age at menarche
endogenous hormones
immune function
insulin resistance
low penetrance genes
However, as you can see there are different lines connecting them, and they differentiate between the strength of association and the research data quality.
Unlike cervical cancer that’s caused by human papilloma virus (HPV), and most incidence of lung cancers are caused by tobacco smoking, the cause of breast cancer isn’t as straightforward.
It’s far more complex.
And here comes the confusing part…
Having one or more risk factors doesn't mean a woman will guarantee to get breast cancer.
And...
Many women who DO develop breast cancer have no obvious risk factors.
How do we make sense of this?
Firstly, I think it’s important to realise that the cause of breast cancer EXTENDS BEYOND these published risk factors.
If you’re at all concerned about preventing breast cancer or if you’ve already been diagnosed you need to understand these risk factors in the context of your own circumstance.
The Real Factors that Causes Breast Cancer
What isn’t explained in great detail is the fact that there is a common underlying reason why these risk factors have been associated with breast cancer.
The majority of these risk factors directly and indirectly relate to oestrogen dominance.
Let’s look at some of these risk factors again:
younger age at onset of menstruation and older age at onset of menopause exposes the woman to a longer duration of circulating oestrogen.
Consuming alcohol impairs the liver to metabolise oestrogen.
Having a high BMI means having a greater amount of fat cells that are able to produce more oestrogen in the body.
Being on the contraceptive pill means adding exogenous oestrogen into the body.
Being on HRT means adding exogenous oestrogen into the body.
Having children earlier on in life and having more than one children is a protective factor, because pregnancy interrupts the levels of oestrogen in the body.
Normal breast cancer cells contain oestrogen receptors and when oestrogen binds to these receptors, it tells the cells to grow. If a breast cell has been damaged by radiation or toxic exposure, having excess oestrogen around will allow the “bad cells” to flourish and grow.
But usually the immune system of young women are able to take out these bad cells. However, when a woman’s immune system becomes weak for long periods of time, these single cancer cells can grow into a tumour.
What’s the association of oestrogen and triple negative breast cancer?
The concern with oestrogen dominance still applies.
Even though oestrogen doesn’t fuel the growth of triple negative breast cancer, you have to remember that before it turned into cancer cell, it was once a normal breast cell with oestrogen receptors.
We also need to educate ourselves about the impacts of toxins, radiation and pollutants on breast health. A woman’s mammary glands are surrounded by fatty tissue. We all know that toxic chemicals accumulate in the blubber of whales and dolphins.
The high levels of toxins that build up in the fatty tissue of the breast which are in close proximity to breast cells initiate the DNA errors that lead to cancer.
What does the complex interplay of risk factors look like in real life?
Let’s take my development of breast cancer as our case study.
Women like myself who have inherited a faulty BRCA-1 or BRCA-2 gene have an impaired DNA repair mechanism in their breast cells.
So how do you explain young women that develop breast cancer who’ve tested negative for any BRCA mutations?
The number of breast cancer associated genes are expanding. Perhaps these women who’ve tested negative do have mutations in several subtle genes. And the likely explanation is that we haven’t identified all the genes responsible for maintaining normal breast cells. There’s no doubt that BRCA-1 and BRCA-2 are the single most important genes identified to date.
However, it’s important to go back to the fundamentals.
There’s more to breast cancer development than one faulty DNA repair enzyme,
What’s often overlooked are the factors that’s driving the DNA errors that transform the breast cell into cancer cells in the first place.
So although I inherited a faulty BRCA-1 gene that’s been associated with a high lifetime risk of breast cancer (~80%), when I was diagnosed, I had no family history of breast cancer.
How can this be when I have a huge family?
Remember that BRCA-1 is a DNA repair enzyme and having a faulty BRCA-1 gene isn’t the proximal cause of breast cancer.
There had to be something in the first place that resulted in DNA damage in one of my original breast cells that finally grew into a tumour in my left breast.
You see, my family migrated to Australia from Indonesia when I was six years old.
So if you compared how I lived and how my relatives lived, there are vast differences in the physical, behavioural and social risk factors for breast cancer.
So could there be factors protecting my female relatives living abroad from breast cancer?
Maybe.
Or has my breast cancer risk factor profile increased dramatically because I grew up and lived here in Australia for many years- and have adopted a more “high-risk” lifestyle?
Most likely.
From migration studies, we can see that the risk of breast cancer in Japanese women living in Hawaii is far higher than that of a Japanese woman in Japan.
Their genetics are the same but because they’ve migrated, their environment has changed.
Prevention isn’t a Dirty Word.
So after much reading and research, one thing is for sure.
There is NO UNIVERSAL CAUSE of breast cancer.
Can you imagine being a scientist and trying to study ONE woman’s genetic, lifestyle and environmental risk of breast cancer. The interplay of risk factors and protective factors could possibly be additive, multiplicative or subtractive.
There would be a dizzying amount of variables to measure and control for.
In other words, each woman’s breast cancer causation profile is going to be a set of genetics, lifestyle and environment factors that is unique to her.
So let’s throw out the notion that any researcher would or could ever study our lives in great detail.
Can we figure out our own risk profile?
I believe we can and we should.
I think the first step is to have a little COURAGE to WANT to understand.
It’s easier to bury our heads in the sand because it’s too scary to really figure this all out.
It’s easier to live a lifestyle and environment that we are use to and comfortable with.
BUT if we’re open to change…
…I believe that those who have had a diagnosis of breast cancer can take reasonable steps to modify their lifestyle and environment so as to prevent a recurrence.
And those that have a strong family history of breast cancer can become more aware and educated as to the cause of breast cancer and feel empowered to prevent breast cancer from ever developing.
Suggested Further Reading: